- About
- Expertise
- Expertise Overview
- De Novo & Disruptive Technologies
- Cadaver Testing & Training
- Physician & Clinical Bio-Skills Training
- Histopathology & Analytical Testing
- Cardiac (Structural Heart & EP)
- Dermal
- Gastrointestinal
- General & Reconstructive Surgery
- Neurological
- Oncology
- Orthopedic/Spine
- Respiratory
- Urogenital
- Vascular
- Wound Healing/Traumatic Injury
- Services
- Testing Services Overview
- Research Models
- GLP Studies & FDA Assistance
- Alprazolam (Xanax)
- Armodafinil (Nuvigil)
- Carisoprodol (Soma)
- Clonazepam (Klonopin)
- Ivermectin (Stromectol)
- Lorazepam (Ativan)
- Modafinil (Provigil)
- Molnupiravir (Lagevrio)
- Prednisone (Deltasone)
- Pregabalin (Lyrica)
- Sumatriptan (Imitrex)
- Testosterone (Cernos)
- Zolpidem (Ambien)
- Zopiclone (Imovane)
- Support
- News/Events
- Blog
- Contact
Preclinical Blog
Considerations for Preclinical Wound Healing Models
Jun 15, 2018
Wound healing is a fundamental process to every living organism. Humans have been tending to each others wounds since the day of our creation. The complexity of human wound care has evolved through history from homemade magical potions, incantations, charms, and ointments to institutionally trained physicians, surgeons, and nurses and an ever increasing industry of wound care products. The industry of wound care products is estimated to reach nearly $21 billion in 2015 (1).
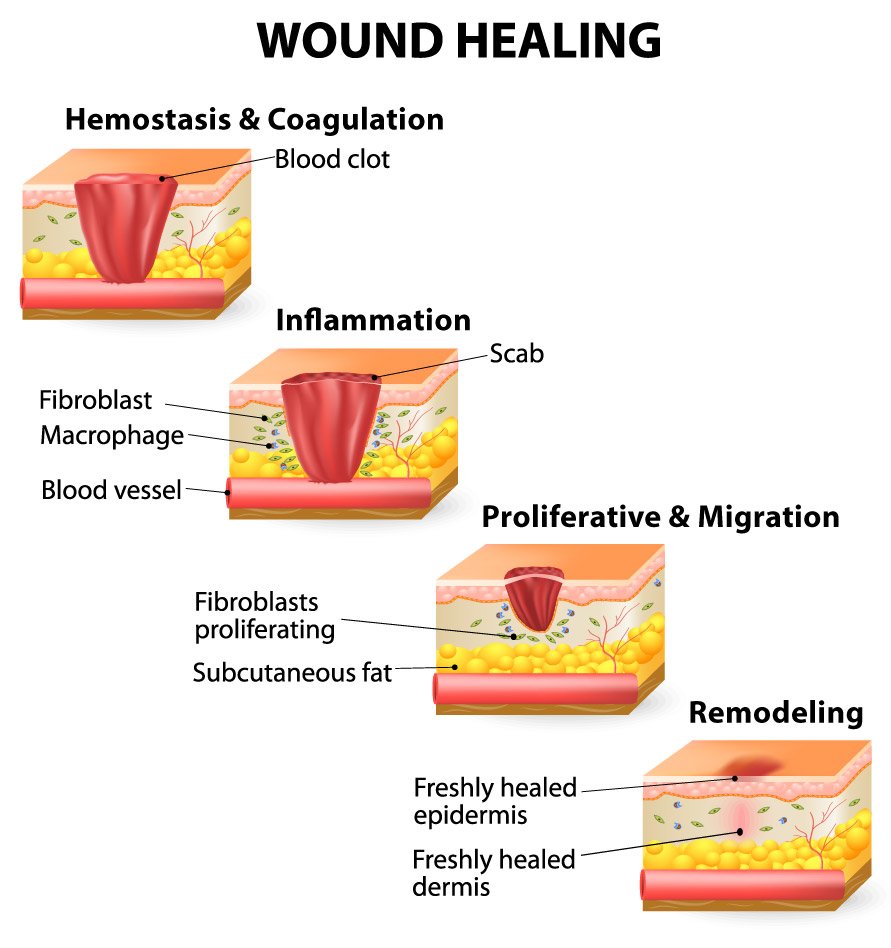
In the surgical environment, a surgeon has to be able to successfully address wounds, both those they create and those they are looking to medically treat. Success in surgery is founded on a comprehensive understanding on the fundamentals of wound healing (2, 3, 4). The outcome of every surgical procedure ultimately depends on the uncomplicated procession through the normal phases of wound healing. Furthermore, to understand the evaluation or development of potential therapeutic products for wound healing in preclinical wound healing models, it is best to begin with appreciation of the mechanisms of wound healing as they apply to most species. The biological processes of wound healing have been described as being as complex as the interplay of musical instruments in a world class orchestra or as the relationships between characters in a multi-book classic literature series (5). The physiologic process of wound healing has traditionally been divided into 3 to 4 distinct biological phases (6, 7, 8): hemostasis and coagulation, inflammation, proliferation and migration, and remodeling. Each of these complex series of reactions involves an ever increasing list of interacting cells and cellular mediators (growth factors and cytokines).
These phases and their biophysiological details must generally take place in sequence and continue for an appropriate duration and intensity to have a good clinical outcome (9). Wounds that demonstrate delayed or impaired healing characteristics generally have failed to progress through the normal phases of healing because of either local or systemic factors (10). Local factors can be described as those factors that directly influence the characteristics of the wound itself (infection, oxygenation, foreign bodies, edema, vascular insufficiency), while systemic factors include those issues associated with the overall health or disease state of the individual that affect their ability to heal (age, level of stress, obesity, medications, smoking, nutrition, status of immune system, diseases).
Animal models of wound healing are important to the process of research and development of clinical therapies for human wound care. Preclinical models provide vital information and insight into the basic mechanisms and physiology of wound progression and healing, as well as provide a platform to evaluate and characterize potential novel products for the treatment of wounds. Many preclinical wound healing models are designed to isolate specific wound phenotypes and mechanisms, however, each preclinical model is ultimately judged by its ability to predict how a treatment will behave in a human wound, under clinical conditions (11). The advantages and disadvantages of each potential wound healing model (including the selection of species, breed, age, gender, wound type, etc.) must be considered in the context of the objective(s) of a preclinical study. Animal models of wound healing should strive for reproducibility, clinical relevance, humane treatment and quantitative interpretation (12).
Surpass has been working with preclinical models of wound healing for more than ten years and our team stands ready as your preclinical partner to consult on appropriate animal models and study design as well as study execution. In addition, the Surpass team will be issuing a series of blog posts on study design for preclinical wound healing studies where we'll walk you through important considerations for your study. Check back to learn more from your preclinical CRO partner, Surpass.
Next Steps
- Sign up to receive notification of future blog posts by Surpass.
- View other blog posts related to Preclinical Study Design.
- Learn more about Surpass' Preclinical Wound Healing Experience.
- Contact us to set up a complimentary scientific consult on your next preclinical wound healing study.
- Download our current Whitepapers on Preclinical In Vivo Study Design and Choosing a Preclinical CRO.





